Vasectomy Reversal
Table of Contents
- Introduction to vasectomy reversal
- Reasons for vasectomy reversal
- Risks associated with vasectomy reversal
- Procedures for vasectomy reversal
- Post-surgical results
- Preoperative factors affecting post-surgical results
Introduction to Vasectomy Reversal
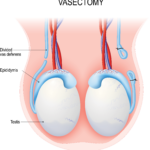
Vasectomy is a contraceptive procedure in which outward passage of sperms used to reach the semen is blocked by cutting, tying, or sealing of vas deferens. 1 It is important to note that you are still producing sperms but not ejaculating them. Vasectomy reversal is a procedure carried out to undo the process of vasectomy. 1,2 It is done by reattaching the two cut ends of vas deferens together or in some cases, by directly attaching vas to the epididymis.
Key Statistics Regarding Vasectomy and Its Reversal
- Vasectomy is a fairly common contraceptive method with about 8% of women relying on it worldwide. 1
- In the United States, approximately 18% of men have a vasectomy done before the age of 45, of which a significant proportion requests to undo the procedure. 3
- Vasectomy reversal restores the fertilizing capability in 80-99.5% of males, however; unassisted pregnancy rates following the surgery are 40-80%. This discrepancy can be explained by the fact that although structurally vasectomy reversal makes genital tract patent, certain biological changes cannot be reversed. 3
What Happens Under Normal Conditions?
Sperms are produced in testes. They undergo a number of modifications before they are able to fertilize an egg. After being produced in testes, they migrate to the epididymis, where they remain till matured. From the epididymis, they enter into the vas deferens, which is a hollow muscular tube. The vas deferens stores mature sperms and transfers them to the urethra via ejaculatory ducts. Ejaculatory ducts are formed by the fusion of seminal vesicles and vas deferens. The seminal vesicles are specialized glands that produce a major portion of the fluid that makes up semen. Thus, before entering the urethra, secretion of seminal vesicles mixes with the mature sperms in ejaculatory ducts. These sperms are then ready to fertilize.
What Happens in a Vasectomy?
In a vasectomy, the vas deferens is cut so that sperms are not able to enter the ejaculatory ducts. However, the secretions from seminal vesicles and other glands are still being produced, so seminal fluid is there for ejaculation but no sperms are present. Moreover, healthy sperms are also being produced, it is just they are not able to reach the semen but instead are soaked up by the body. Therefore, vasectomy reversal can help in becoming fertile again.
Reasons for Vasectomy Reversal
Vasectomy reversal is usually done for emotional reasons 3 or because of a medical condition. These include:
- Loss of a child
- Starting a new relationship
- Change of mind and wanting to increase family
- Persistent pain following vasectomy 4
The pain may be present on one or both sides and may occur with intercourse or during physical activity. Several causes can be attributed to this pain: 4
- Hematoma formation may occur at the site of surgery. Hematoma is an accumulation of blood because of a leaky vessel.
- Postoperative infection can be another cause.
- Sometimes during surgery, a nerve may impinge. It will constantly carry pain signals to the higher centers, resulting in persistent pain.
- Our organs lie in the body in different sacs along with their blood vessels, nerves, and all surrounding and supporting structures. When the contents of these sacs leak, it is called a hernia. After a vasectomy, contents of the inguinal canal (vas deferens and other important reproductive structures) may leak causing pain.
- Other causes could be testicular neoplasm or pain of psychogenic origin.
Risks Associated with Vasectomy Reversal
Vasectomy reversal is a minor surgery that can be safely done in outpatient settings or Ambulatory Surgery Centers with minimum complications. However, just like any other surgery, there are some risks associated with this surgery too. These are:
- Scrotal hematoma: Sometimes, there is severe bleeding after surgery. The blood accumulates within the scrotum. The scrotum is a bag-like structure that holds the testes. It is maybe displeasing and painful for the patient.
- Postoperative infection: Infection at the site of surgery can occur because of a lacerated wound that allows the microorganisms to enter the site. A course of antibiotics is, therefore, prescribed by your doctor to decrease the risk of any infection.
- Mild to severe scrotal pain: Pain may occur because of the surgical procedure. It may last for a few weeks and can be controlled with analgesics. Some patients report the pain to be similar to what was experienced following vasectomy.
- Stricture formation: Stricture, in medical terms, means obstruction of a tube-like structure. Vas deferens is a very narrow, delicate tube. After it is rejoined, the body’s immune system may become activated. The immune cells may accumulate forming a group, resulting in the formation of a small obstruction called a stricture.
Procedures for Vasectomy Reversal
Vasectomy reversal is a minor but complex surgical procedure carried out under anesthesia. The choice of anesthesia depends on the patient. 2 General anesthesia is when you are in a deep sleep, completely unconscious of your surroundings. Local anesthesia is when only the sensations in your lower abdominal region are blocked and you are awake, completely aware of what is happening around you. Before surgery, your doctor will discuss all surgical options, the procedure, chances of pregnancy following them, and any possible risk.
Generally. the preferred procedure for vasectomy reversal is microscopic surgery or microsurgery. 2 In this, the surgeon uses a high-power microscope to magnify the tiny tubes and create a better image for better performance. The stitches used are very delicate in order to minimize any possible iatrogenic damage. The surgical procedure starts with a small incision on both sides of the scrotum.
Before initiating the process of vasectomy reversal, your surgeon will check for the presence of sperms in the remaining part of vas deferens that is connected to the testes. For this purpose, they will obtain some fluid from the testicles. Depending upon the existence of sperms, the surgeon will opt for one of the following options to undo vasectomy:
Vasovasostomy:
In this procedure, both ends of vas deferens are stitched together. It is done if the sperms are present in the vasal fluid (fluid obtained from the vas deferens.) The presence of sperms depicts that the path of the sperms from testes to vas deferens is patent, so it can be carried out safely and effectively.
Vasoepididyostomy:
If there are no sperms in the vasal fluid, then it means that during the vasectomy, the path was either destroyed or blocked. Your surgeon will now directly connect the patent portion of vas deferens with epididymis. This procedure is called vasoepididymostomy, which means connecting vas deferens and epididymis.
Vasoepididymostomy is a more complex procedure than vasovasostomy. Your doctor may perform vasovasostomy one side and vasoepididymostomy on the other, depending upon the presence of the sperms in vasal fluid, obtained from either side.
Post-surgical Results
Healing:
The healing usually occurs quickly and easily without any major complication. Pain is a common complaint that can be easily resolved with pills. The severity of pain may vary in different individuals. Daily routine activities can be started within a week of surgery. It is best to avoid sex for 2-3 weeks following vasectomy reversal so that complete healing is ensured.
Fertility:
Following surgery, your doctor will keep on checking the number of sperms appearing in semen. Usually, the sperm count becomes normal in 3-6 months. It is recommended to get a semen analysis done every three months or until pregnancy is achieved for monitoring fertility. 5
Success rate:
Vasovasostomy is a highly successful operation in restoring structural patency. With modern microsurgical techniques, 80-100% patency can be achieved with vasovasostomy. 6 The patency rate achieved with vasoepididymostomy, however, is between 50-85%. 7
Failure rate:
It is estimated that about 30% of all vasectomy reversal procedures fail. The reason is either ineffective vasal anastomosis (joining of vassal ends) or some other unrecognized obstruction. 8 Usually, if the sperms do not appear within six months, it is considered that the vasectomy reversal has failed. 9
What Happens When the First Attempt at Vasectomy Reversal Fails?
Vasectomy reversal failure is often seen on the first attempt but it does not mean you cannot father a child. The following options are available if the first attempt at vasectomy reversal fails:
- Second attempt at vasectomy reversal: For many, a second attempt at vasectomy removal can produce desirable results. It is seen that microsurgical reconstruction following vasectomy reversal failure is associated with high anatomical patency rate and moderate pregnancy rate. 8
- Frozen sperm: In case a second attempt also fails, using frozen sperm is another option available. In this method, sperms are obtained directly from the testes and are stored in viable conditions. They can later be placed into the uterus through in vitro fertilization when the egg is available.
Preoperative Factors Affecting Post-Surgical Results
There are certain factors that result in deterring the success rate of fertility and conception following vasectomy reversal. 10 These are:
- The duration between vasectomy and vasectomy reversal: The appearance of sperms in semen following vasectomy reversal surgery is greatly influenced by the duration between the two surgical procedures. The greater the duration, the lesser the sperm quantity and quality. 11
- Sperm granuloma: After a vasectomy, sometimes, a small mass is formed in the epididymis obstructing it. It is a result of the body’s immune reaction to sperms leaking from the cut end of vas deferens.
- Previous healthy sperms: The failure of the procedure can also be seen if the man was producing unhealthy sperms even before vasectomy. It is important to check the previous fertility status of those who have not had any child before.
- Quality of vasal fluid: If there is only a sperm head or sperm tail found in the vasal fluid, the choice of correct surgical procedure becomes difficult.
- Microsurgical technique: The surgical technique used is another factor crucial for fertility. It is important to minimize the risk of the iatrogenic defect. The results are good when the microsurgical technique is used.
- Age and fertility status of the partner: The fertility status of the partner is essential for conception. If your partner has some gynecological issues, this may also interfere with conceiving. The age of the female partner is also important. Fertility generally declines with age. At menopause, eggs are no longer there and a female cannot reproduce.
References:
- Pile, J. M., & Barone, M. A. (2009). Demographics of vasectomy–USA and international. The Urologic clinics of North America, 36(3), 295–305.
- Belker A. M. (1987). Vasectomy reversal. The Urologic clinics of North America, 14(1), 155–166.
- Bernie, A. M., Osterberg, E. C., Stahl, P. J., Ramasamy, R., & Goldstein, M. (2012). Vasectomy reversal in humans. Spermatogenesis, 2(4), 273–278.
- Smith-Harrison, L. I., & Smith, R. P. (2017). Vasectomy reversal for post-vasectomy pain syndrome. Translational andrology and urology, 6(Suppl 1), S10–S13.
- Bolduc, S., Fischer, M. A., Deceuninck, G., & Thabet, M. (2007). Factors predicting overall success: a review of 747 microsurgical vasovasostomies. Canadian Urological Association journal = Journal de l’Association des urologues du Canada, 1(4), 388–394.
- Yarbro, E. S., & Howards, S. S. (1987). Vasovasostomy. The Urologic clinics of North America, 14(3), 515–526.
- Chan P. T. (2013). The evolution and refinement of vasoepididymostomy techniques. Asian journal of andrology, 15(1), 49–55. https://doi.org/10.1038/aja.2012.80
- Hernandez, J., & Sabanegh, E. S. (1999). Repeat vasectomy reversal after initial failure: overall results and predictors for success. The Journal of urology, 161(4), 1153–1156.
- Jarow, J. P., Sigman, M., Buch, J. P., & Oates, R. D. (1995). Delayed appearance of sperm after end-to-side vasoepididymostomy. The Journal of urology, 153(4), 1156–1158.
- Ramasamy, R., & Schlegel, P. N. (2011). Vasectomy and vasectomy reversal: An update. Indian journal of urology : IJU : journal of the Urological Society of India, 27(1), 92–97.
- Shin, Y. S., Kim, S. D., & Park, J. K. (2012). Preoperative factors influencing postoperative results after vasovasostomy. The world journal of men’s health, 30(3), 177–182.